Question #1
A 58-year-old man is brought to the emergency department because of weakness of the right arm and face and an inability to speak. He has a history of alcohol use, cigarette smoking, and hypertension. Neurologic examination shows an alert mental status. He is only able to say a few words with great effort, is unable to repeat, but can follow simple commands. He has a decreased right nasolabial fold and decreased movements of his right face, sparing the forehead. He has no right arm movement, but is able to raise his right leg.
Occlusion of which of the following blood vessels best explains the findings in this patient?
Left anterior cerebral artery
Left middle cerebral artery
Posterior cerebral artery
Posterior inferior cerebellar artery
Right anterior cerebral artery
Right middle cerebral artery
Answer:
The correct answer is B.
Because this patient has right-sided motor symptoms, choices E and F can be immediately eliminated because contralateral motor symptoms should result. There is no discussion of visual field defects that would occur with a lesion of the visual cortex, eliminating choice C. Lateral medullary (Wallenberg) syndrome (see below), which occurs with PICA strokes, is not evident, ruling out choice D. This leaves us with choices A and B. His arm is affected and his leg is spared (ruling out choice A); he also has Broca's aphasia. This indicates a stroke of the lateral language-dominant cortex, which is supplied by the left middle cerebral artery (choice B). We have quickly arrived at the correct answer, but let's review the neuroanatomy in more detail.
This patient most likely had a stroke of the left middle cerebral artery. This artery supplies the lateral surface of the frontal, parietal, and upper temporal lobes; the internal capsule; and most of the basal ganglia. The MCA is the vessel that is most commonly affected by cerebrovascular accidents and can result in:
Spastic paresis of the contralateral lower face and upper limb (the upper face is spared because of the bilateral upper motor neuron innervation of the facial nucleus that innervates the upper face)
Anesthesia of the contralateral face and upper limb
Aphasia (e.g., Broca's or Wernicke's) if the stroke occurred in the language-dominant hemisphere
Hemineglect if the stroke occurred in the nondominant hemisphere
The symptoms produced by an MCA occlusion can vary depending on the size and location of the thrombus.
This patient has Broca aphasia, which can result when branches of the left MCA that supply Broca's area in the inferior frontal gyrus, are occluded in the language-dominant (usually left) hemisphere. Broca aphasia is characterized by slow, nonfluent speech with deficits in word finding ("broken" aphasia). Because comprehension is normal (patients are able to follow commands), they are typically aware of the problem and can be very frustrated. Repetition, writing, and reading aloud is impaired, but reading comprehension is often relatively preserved. This is in contrast to Wernicke aphasia, in which speech is nonsensical, but fluent ("word salad"), and the patient has a lack of both comprehension and awareness of his or her syndrome.
This patient also has right lower facial weakness and right arm weakness. The figure below shows the close proximity of Broca's area to the lateral part of primary motor cortex, demonstrating why these symptoms often appear together.
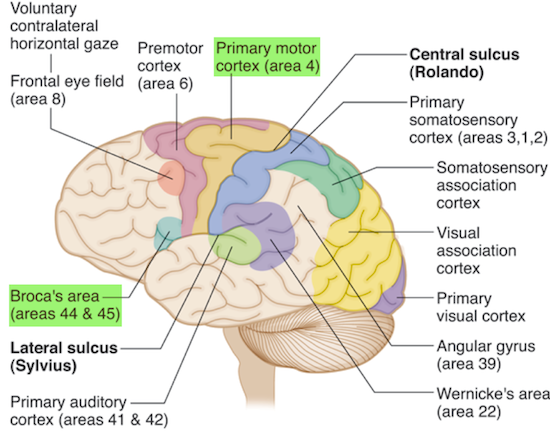
The figure below shows the motor homunculus, demonstrating why the upper limb and face is preferentially affected with an MCA stroke.
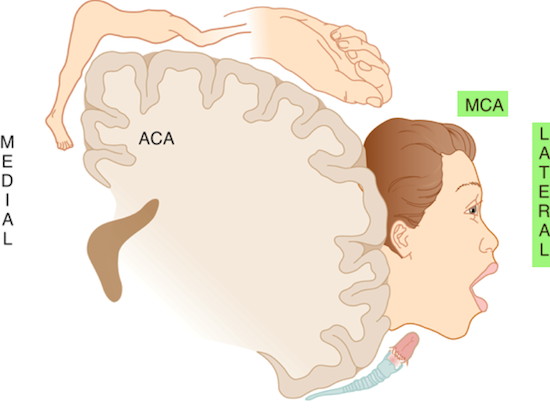
The anterior cerebral arteries (ACAs) (choices A and E) supply the medial surface of the frontal and parietal lobes, which include motor and sensory cortical areas of the pelvis and lower limbs. ACA occlusion results in spastic paresis and anesthesia of the contralateral lower limb. Urinary incontinence may be present (usually occurs with bilateral damage).
The posterior cerebral artery (choice C) supplies the occipital lobe, the thalamus, and part of the temporal lobe. Occlusion of this artery results in a homonymous hemianopia of the contralateral visual field with macular sparing.
The posterior inferior cerebellar artery (PICA) (choice D) supplies the lateral medulla. Occlusion of the PICA leads to Wallenberg syndrome (lateral medullary syndrome). These patients present with ipsilateral limb ataxia, ipsilateral loss of pain and temperature sensation of the face, contralateral loss of pain and temperature sensation of the body, ipsilateral Horner syndrome (ptosis, miosis, anhidrosis), hoarseness, dysphagia, nausea and vomiting, vertigo, and nystagmus.
Most individuals are left hemisphere–dominant. When the right MCA (choice F) is affected (i.e., the nondominant hemisphere), patients present with left-sided neglect (asomatognosia) in which they are unaware of the contralateral (left) side of their bodies. These patients fail to dress, undress, or wash the affected side. In addition, a stroke of the right MCA would produce left lower facial and arm weakness, unlike the right-sided motor deficits of this patient.
Question #2
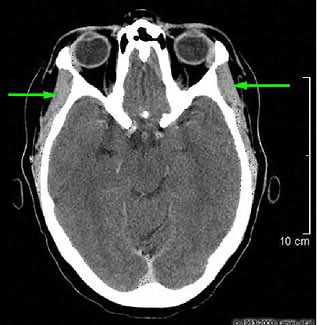
A 79-year-old man comes to the physician because he has been "bumping into walls and objects," especially on his right side. He says that his symptoms began suddenly upon awakening last week and that wearing glasses did not help. He does not have vertigo or dizziness, and has had no loss of consciousness, lightheadedness, or tinnitus. Examination shows pupils are approximately 4 mm, equal, round, and react normally to light and accommodation. His extraocular movements are all intact. He has a corrected visual acuity of 20/20 in both eyes. However, visual fields are reduced on the right side in both eyes.
Occlusion of which of the following blood vessels is most likely responsible for this patient's symptoms?
Anterior communicating artery
Internal carotid artery
Middle cerebral artery
Ophthalmic artery
Posterior cerebral artery
Posterior communicating artery
Vertebral artery
Answer:
The correct answer is E.
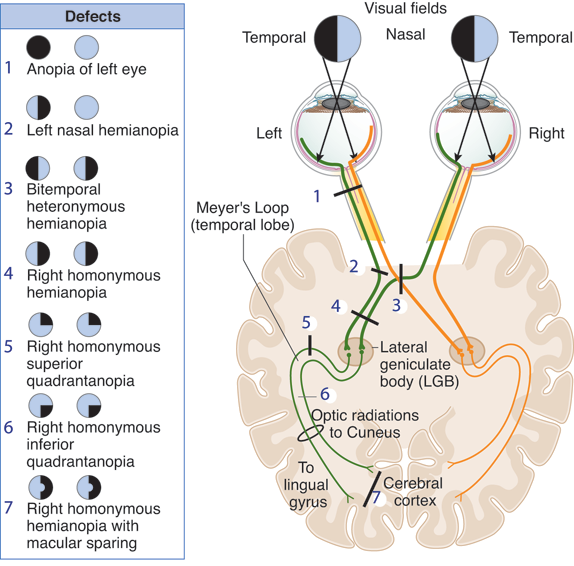
This patient has most likely undergone a left posterior cerebral artery (PCA) stroke, resulting in a right homonymous hemianopsia. Extensive visual field testing will show macular sparing. Since many individuals associate stroke with motor weakness or language loss, they may often avoid seeking immediate medical attention after experiencing only visual changes. The PCA supplies the occipital cortex, where the primary visual cortex is located.
Infarction of this region in one hemisphere will produce a homonymous hemianopsia. However, unlike injury to the lateral geniculate nucleus or the optic radiations, the blood supply in the most posterior region of the occipital cortex, where the macula is represented, is bilaterally redundant. As a result, occipital lobe strokes often spare the macula, and hence visual acuity is preserved, as in this patient. The distribution of the posterior, middle, and anterior cerebral arteries is shown below.
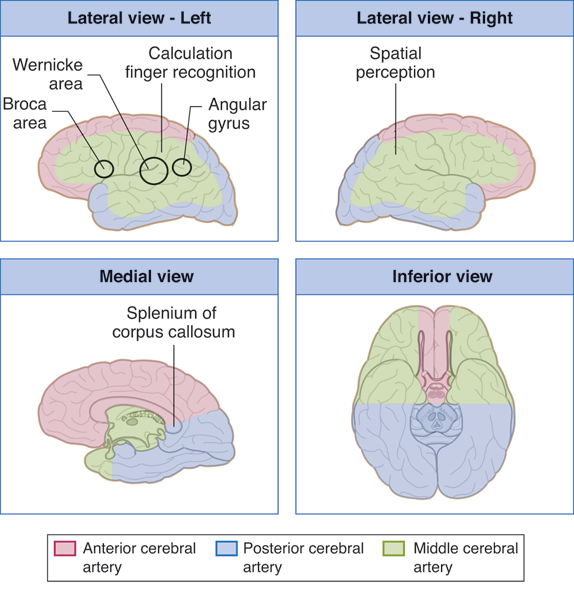
The anterior communicating artery (choice A) is located in the vicinity of the optic chiasm. Aneurysms in this blood vessel may impinge on crossing fibers to cause a bitemporal hemianopsia.
The internal carotid artery (choice B) gives rise to the ophthalmic arteries as well as the anterior circulation of the cortex. An infarct in this location would produce a much more dramatic effect than the one this patient experienced. Calcification of the internal carotid arteries in the vicinity of the optic chiasm can lead to binasal hemianopsia.
The middle cerebral artery (choice C) is a common location for strokes. Since it supplies a major portion of the parietal cortex as well as the motor strip, patients usually experience a hemiparesis, with language dysfunction if the stroke occurs in the language-dominant hemisphere. The middle cerebral artery perfuses the primary motor and primary sensory cortices responsible for the upper extremities and head region (which can be seen in a homunculus of these regions).
The ophthalmic artery (choice D) perfuses the optic nerve as well as the retina. However, an occlusion of this artery would lead to monocular blindness, not a visual field defect.
The posterior communicating arteries (choice F) overlie CN III (oculomotor nerve). Therefore, aneurysms of these arteries can often lead to a third-nerve palsy, resulting in strabismus, with the affected eye primarily pointed downward and outward on primary gaze.
Vertebral arteries (choice G) provide much of the posterior circulation for the brain stem and cerebellum. Strokes from these vessels will not produce a visual field defect, but can produce signs of brain stem and/or cerebellar dysfunction. Medial medullary syndrome can be caused by occlusion of the vertebral or anterior spinal arteries.
The table below summarizes visual deficits due to arterial pathology (e.g., occlusion, aneurysm, calcification), which is highly tested on the USMLE.
Question #3
A 58-year-old man comes to the physician because of recurrent headaches and ear pain. The pain worsens with chewing and yawning. Occasionally, the patient also notices a "clicking sensation" near his ear while chewing. On physical examination, firm palpation below the ear reproduces the pain. The structures indicated by the arrows on this CT scan are tender to palpation.
Which of the following is the most likely location of the cranial nerve nuclei that provide motor innervation to the indicated structures?
Lower pons
Medulla
Midbrain
Mid-pons
Spinal Cord
Answer:
The correct answer is D.
This patient has temporomandibular joint syndrome (TMJ). Common symptoms include chronic pain in the muscles of mastication, pain that can radiate to the ear and is worse when chewing, ear clicking or popping, headache, and locking of the jaw when attempting to open the mouth.
The muscle indicated on the CT scan is the temporalis muscle, one of the muscles of mastication (the others are the masseter, the lateral pterygoid and the medial pterygoid muscles). It is innervated by cranial nerve V, the trigeminal nerve. The trigeminal nerve has three major branches: ophthalmic, maxillary, and mandibular. The ophthalmic and maxillary nerves are purely sensory. The mandibular nerve has both sensory and motor functions. The motor nucleus of cranial nerve V is located in the mid-pons. This nucleus, in addition to innervating muscles of mastication, also supplies the tensor tympani, the mylohyoid, and the anterior belly of the digastric.
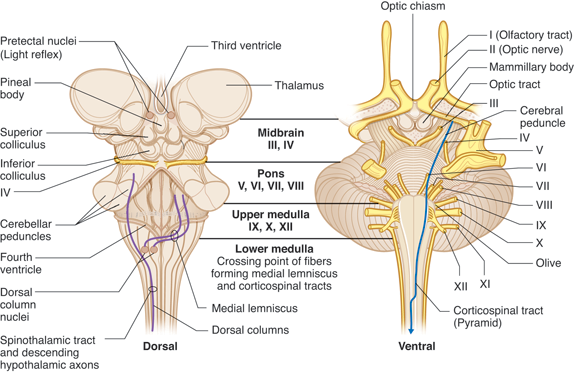
The lower pons (choice A) contains the facial nucleus, which gives rise to the motor fibers of the facial nerve and innervates muscles of facial expression and the stapedius, stylohyoid, and posterior belly of the digastric muscles.
The medulla (choice B) contains the motor nucleus for cranial nerves IX (innervates the stylopharyngeus muscle), X (innervates muscles of the larynx and pharynx), XI (supplements the vagus nerve), and XII (innervates the extrinsic and intrinsic muscles of the tongue except the palatoglossus muscle).
The midbrain (choice C) contains the oculomotor nucleus, which innervates the medial rectus, superior rectus, inferior rectus, and inferior oblique extraocular muscles as well as the levator palpebrae superioris muscle (elevates the upper eyelid).
The spinal division of CN XI arises from C1 through C6 of the spinal cord (choice E) and innervates the sternocleidomastoid and trapezius muscles.
Question #4
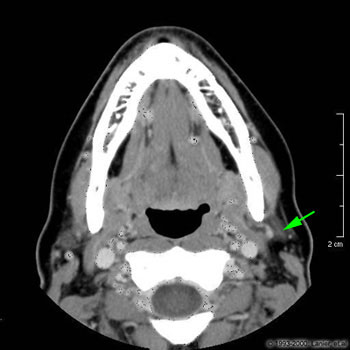
An 18-year-old man is brought to the emergency department after sustaining injuries to the left side of his face during a bar fight. Physical examination shows a deep, 10-cm laceration obliquely across the left cheek. The man cannot shut his left eye and cannot smile on the left side of the face. A normal CT of the head is shown.
Which of the following additional structures in the normal CT indicated by the arrow is most likely damaged?
Common carotid artery
Masseter
Parotid gland
Sublingual gland
Temporalis
Answer:
The correct answer is C.
This head CT shows the parotid gland, which covers the masseter muscle, extends posteriorly beyond the vertical ramus of the mandible, and abuts the external auditory meatus. The parotid gland is traversed by the facial nerve as it travels toward the muscles of facial expression. Injury to this nerve accounts for the patient's inability to close the eye or smile on the side of the laceration. Injury to the facial nerve is a significant risk during parotid surgery.
The common carotid artery (choice A) does not pass through the area of injury. The common carotid artery bifurcates at about the level of the C3-C4 vertebra, well below the level of the mandible and below the level of this CT. The external carotid artery, however, does pass through the parotid gland.
The masseter muscle (choice B) is a muscle of mastication, and is thus innervated by cranial nerve V. It can be seen in this CT anterior to the parotid gland and on the lateral surface of the mandible.
The sublingual gland (choice D) is located in the anterior portion of the floor of the mouth, not on the lateral side of the face.
The temporalis muscle (choice E) is also a muscle of mastication innervated by cranial nerve V. It inserts on the coronoid process of the mandible, superior to the level of this CT, and therefore cannot be seen on this CT.
Question #5
A 17-year-old boy is brought to the emergency department because of an "arm and shoulder injury" that occurred during a baseball game. He says that he was standing on the sideline when he suddenly got hit in the right upper arm and shoulder with a batted ball. An x-ray of the shoulder shows a fracture of the surgical neck of the humerus.
Which of the following will most likely be seen in this patient?
Laceration of the profunda brachii artery
Weakness in medial rotation of the arm
Weakness in the ability to abduct the arm at the shoulder
Weakness in the ability to elevate the scapula
Weakness in the ability to protract the scapula
Answer:
The correct answer is C.
This patient most likely has an injury involving the axillary nerve, which may be injured by a blow near the shoulder joint. This nerve innervates the deltoid muscle and the teres minor. The clinical features of injury to this nerve include weakness of shoulder abduction and a sensory loss in the upper arm and shoulder.
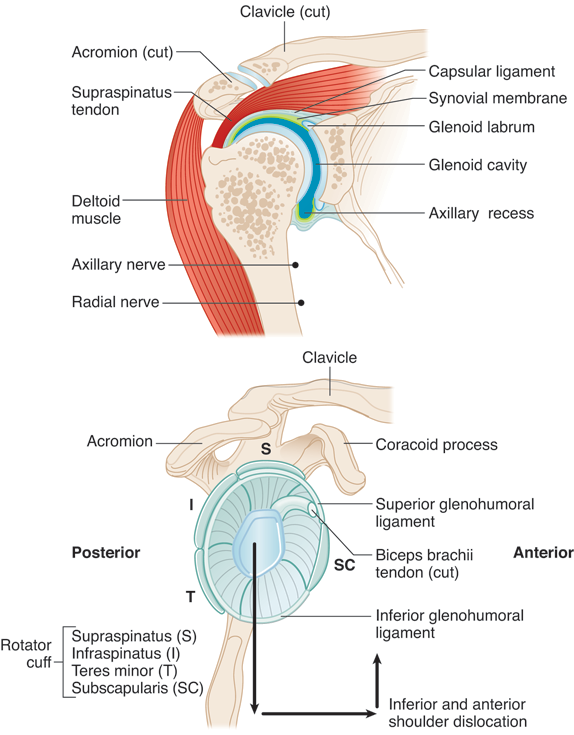
Laceration of the profunda brachii artery (choice A) might occur if one suffers a midshaft fracture of the humerus; a surgical neck fracture may lacerate the posterior circumflex humeral artery instead.
Weakness in medial rotation of the arm (choice B) may result from a lesion to the posterior cord of the plexus and one or more of the subscapular nerves.
Weakness in the ability to elevate the scapula (choice D) may result from a lesion of the accessory nerve; this nerve may be lacerated by stab wounds to the lateral neck, but not by a humeral fracture.
Weakness in the ability to protract the scapula (choice E) results from an injury to the long thoracic nerve, which innervates the serratus anterior muscle, causing "winging" of the scapula. This presents as protrusion of the scapula when the patient pushes against a wall. There will be no sensory deficits.
Now that you've tasted a few questions, are you ready for more?
Enroll in our Step 1 Qbank and practice with over 2,000 USMLE-style questions, now with a lower price. Start now with our Until Your Test® access and get a higher score.
Fill out the information below to get the answers and explanations. We’ll also email you free tips, admissions advice, exclusive offers, and other content aimed specifically to help you do better on Test Day.